Everything You Need To Know About Chronic Obstructive Pulmonary Disease (COPD)

Welcome to our comprehensive guide on everything you need to know about Chronic Obstructive Pulmonary Disease (COPD).
As a team dedicated to serving others, we understand the importance of providing accurate and helpful information about this progressive lung disease.
This article will explore the early symptoms, worsening signs, causes, prevention strategies, and more.
We aim to empower you with knowledge so chronic obstructive pulmonary disease can be effectively managed, so we may live life to its fullest potential.
Key Takeaways
COPD is a progressive lung disease that includes chronic bronchitis and emphysema.
The primary cause of COPD is cigarette smoking, although not all smokers develop the disease.
Risk factors for COPD include gender, age, exposure to pollutants, certain occupations, and genetic factors.
Symptoms of COPD include cough with mucus, difficulty breathing, wheezing, and shortness of breath during exercise and daily activities.
Commonly Prescribed Medications
Early symptoms
Early symptoms of COPD, such as occasional shortness of breath and a mild cough, can be mistaken for a cold. It is important to recognize these signs and seek medical attention if they persist or worsen.
Chronic obstructive pulmonary disease is a progressive lung condition affecting millions worldwide. These early symptoms may seem minor at first but should not be ignored. If you find yourself experiencing intermittent coughing, wheezing, chest tightness, or difficulty breathing during physical exertion, it could indicate COPD.
Be sure to seek help from healthcare professionals who can provide an accurate diagnosis and appropriate treatment options before the symptoms worsen.
Now let's explore the worsening symptoms of COPD and how they can impact your daily life.
Worsening symptoms
As COPD progresses, symptoms worsen, including more frequent and severe episodes of shortness of breath, chronic coughing, wheezing, and recurring respiratory infections. These worsening symptoms can greatly impact daily life and reduce overall .
It is important to understand that COPD is a progressive disease and its severity can be classified into four stages based on spirometry testing. Early intervention and appropriate treatment are crucial in managing the progression of the disease.
Treatment options for COPD aim to alleviate symptoms, slow down the progression of the disease, and improve overall lung function. This may involve medications such as bronchodilators and glucocorticosteroids, oxygen therapy if blood oxygen levels are low, lifestyle changes like quitting smoking, maintaining a healthy diet, regular exercise, weight management, and vaccination against respiratory infections.
These interventions can help in managing the worsening symptoms effectively.
Now let's discuss the signs and symptoms associated with COPD.
Signs and symptoms
When COPD progresses, you will experience worsening symptoms such as frequent and severe shortness of breath, chronic coughing, wheezing, and recurring respiratory infections. These symptoms can greatly impact your daily life and make engaging in activities you once enjoyed difficult. It's important to recognize these signs and seek medical attention for proper diagnosis and management of COPD.
To help you understand the progression of COPD, here is a table that illustrates the stages of COPD:
Stage | Description | Symptoms |
|---|---|---|
Mild | Early stage with mild airflow limitation | Occasional shortness of breath, mild cough |
Moderate | Increased airflow limitation | Shortness of breath with moderate exercise |
Severe | Significant airflow limitation | Chronic cough, frequent respiratory infections |
Very Severe | Severe airflow limitation requiring medical care | Severe shortness of breath even at rest |
As COPD progresses through these stages, the severity of symptoms worsens. It's crucial to be aware of these signs so that appropriate steps can be taken for effective management.
Now, let's discuss what causes COPD (chronic obstructive pulmonary disease).
What causes COPD (chronic obstructive pulmonary disease)?
The main cause of COPD is long-term exposure to irritants, primarily cigarette smoke. Tobacco smoke is the leading risk factor for developing COPD, although not all smokers will develop the disease. Other irritants that can contribute to COPD include secondhand smoke, air pollution, and chemical fumes. There is also a rare genetic condition called alpha-1 antitrypsin deficiency that can increase the risk of developing COPD. It's important to note that these irritants cause lung damage over time, leading to the characteristic symptoms of COPD.
A diagnosis of COPD involves evaluating medical history, conducting a physical exam, and performing diagnostic tests such as spirometry to assess lung function. Understanding what causes COPD helps identify preventative measures and manage the disease effectively.
Moving on to chronic bronchitis...
Chronic bronchitis
Chronic bronchitis is characterized by constant irritation and inflammation of the airway lining, leading to symptoms such as persistent cough with mucus production. It is one of the main types of COPD.
It can be diagnosed through medical history, lung function tests, and other diagnostic procedures. There are four stages for COPD based on spirometry testing, ranging from mild to severe.
In the early stages, symptoms may be mild and infrequent, but as the disease progresses, symptoms worsen and become more frequent. It's important to seek medical attention if you experience any symptoms or have been diagnosed with COPD to receive appropriate treatment and management strategies.
Moving forward into the next section about 'other causes', it is crucial to understand other factors that contribute to the development of COPD.
Other causes
Now let's talk about other causes of chronic obstructive pulmonary disease (COPD). While smoking is the primary cause, there are other factors that can contribute to the development of COPD. Here are three important things to know:
Exposure to secondhand smoke; being around people who smoke increases your risk of developing COPD.
Occupational exposure; certain jobs, such as mining or construction, expose individuals to harmful particles and chemicals that can damage the lungs over time.
Genetic factors; in some cases, COPD is caused by genetic factors like alpha-1 antitrypsin deficiency.
Understanding these additional causes of COPD helps us understand the complexity of the condition. It's important to note that COPD progresses through stages, with each stage representing a different level of lung function impairment.
Next, we will discuss how COPD is diagnosed and the steps involved in determining its severity.
How is COPD (chronic obstructive pulmonary disease) diagnosed?
Healthcare providers typically evaluate a person's medical history, conduct a physical examination, and perform lung function tests to diagnose COPD. These diagnostic measures help determine the presence and severity of COPD. The medical history assessment involves discussing symptoms, exposure to risk factors such as smoking or occupational hazards, and any family history of lung disease. During the physical examination, healthcare providers listen to the lungs with a stethoscope and assess overall respiratory function. Lung function tests, such as spirometry, measure how much air a person can inhale and exhale and how quickly they can do so. This helps determine if there is airflow obstruction present in the lungs. Additionally, chest X-rays or CT scans may be done to assess lung damage or rule out other conditions.
Diagnostic Measures | Description |
|---|---|
Medical History Assessment | Discussing symptoms, risk factors (smoking), family history |
Physical Examination | Listening to the lungs with a stethoscope |
Lung Function Tests (Spirometry) | Measuring inhalation/exhalation capacity and speed |
Now, let's explore how chronic obstructive pulmonary disease is managed.
How is chronic obstructive pulmonary disease managed?
Managing COPD involves lifestyle changes, medications, and therapies to alleviate symptoms and slow disease progression. The stages of COPD, which are determined through spirometry testing, play a crucial role in guiding the management approach.
In the early stages, lifestyle modifications such as quitting smoking, avoiding lung irritants, and maintaining a healthy diet are essential. Medications like bronchodilators and glucocorticosteroids can help reduce symptoms and prevent flare-ups.
Pulmonary rehabilitation programs provide education on effective breathing techniques and offer support for managing daily activities with COPD. These steps can greatly improve the quality of life of individuals with COPD.
Lifestyle changes
Start making lifestyle changes to manage your COPD better. Lifestyle modifications can greatly improve your quality of life and help slow down the progression of the disease. Here are some key changes you can make:
Quit smoking; if you haven't already, quitting smoking is crucial for managing COPD. Smoking worsens symptoms and accelerates lung damage.
Exercise regularly; engaging in regular physical activity, such as walking or swimming, can strengthen your respiratory muscles and improve lung function.
Maintain a healthy diet; eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health and provide essential nutrients for lung function.
By incorporating these lifestyle changes into your daily routine, you can take control of your COPD management. The next section will discuss the importance of exams and tests in diagnosing and monitoring COPD progression.
Exam and tests
To better understand and manage your condition, it's important to undergo exams and tests to diagnose and monitor the progression of COPD. These exams and tests play a crucial role in determining the severity of your COPD, identifying any complications or comorbidities, and guiding treatment decisions.
Here are some common exams and tests you may need:
Spirometry: This test measures how much air you can breathe in and out and how fast you can exhale. It helps determine the presence and severity of airflow limitation.
Chest X-ray: This imaging test allows doctors to visualize your lungs, heart, and chest structures. It can help identify lung abnormalities or complications.
Arterial blood gas (ABG) test: This test measures oxygen and carbon dioxide levels in your blood. It helps assess lung function and determine the need for supplemental oxygen therapy.
After these exams and tests, your healthcare provider can provide personalized treatment recommendations based on your specific condition.
Now let's move on to discussing emphysematous destruction and small airway inflammation.
Emphysematous destruction and small airway inflammation
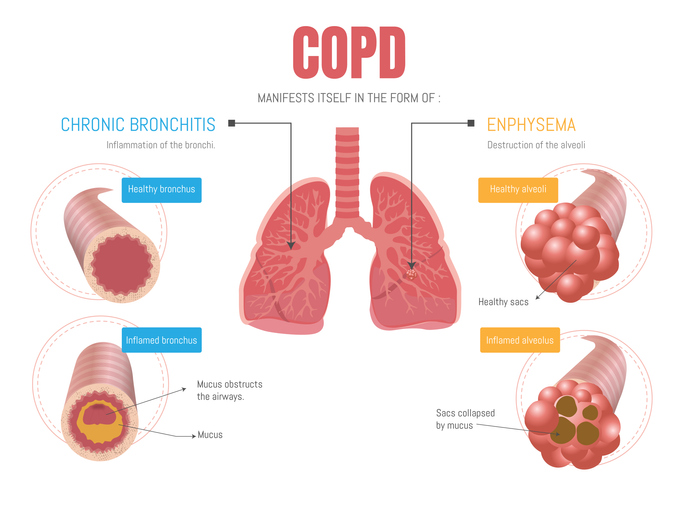
Emphysematous destruction and small airway inflammation contribute to the progression of COPD. In emphysema, the destruction of the air sacs in the lungs leads to a loss of elasticity and reduced airflow. This makes it difficult for oxygen to enter the bloodstream and for carbon dioxide to be expelled.
Additionally, chronic inflammation of the small airways in COPD results in narrowing and mucus production, further obstructing airflow. These processes lead to persistent shortness of breath, coughing, and wheezing experienced by individuals with COPD.
Moving forward to our discussion on alpha-1 antitrypsin (AAT) deficiency, it is worth noting that this genetic condition can also contribute to the development of COPD.
AAT deficiency
AAT deficiency is a genetic condition that can contribute to the development of COPD. It occurs when there is a lack or dysfunction of alpha-1 antitrypsin, a protein that protects the lungs from damage caused by enzymes released during inflammation.
Without enough alpha-1 antitrypsin, these enzymes can destroy lung tissue and lead to the development of emphysema, one of the main types of COPD.
AAT deficiency is relatively rare, but it increases the risk of developing COPD at an earlier age, especially in individuals who smoke or have been exposed to other lung irritants.
If you have symptoms of COPD, such as persistent coughing, shortness of breath, or wheezing, it is important to call your healthcare provider for further evaluation and diagnosis.
When should I call my healthcare provider if I have COPD symptoms?
If you experience symptoms like persistent coughing, shortness of breath, or wheezing, it's important to reach out to your healthcare provider. They can evaluate your symptoms and determine the best course of action. Your healthcare provider may recommend further testing, such as spirometry or imaging tests, to confirm a diagnosis of COPD. Paying attention to these symptoms is essential, as early intervention can help manage the condition and improve your quality of life.
In particular, if your shortness of breath has worsened or occurs more often, you must contact your healthcare provider promptly. This change in symptom severity may indicate a worsening of COPD and require adjustments in your treatment plan. Don't hesitate to seek medical attention and communicate any changes in your condition with your healthcare team for appropriate guidance and support.
Shortness of breath that has become worse or occurs more often
When shortness of breath worsens or occurs more frequently, you must contact your healthcare provider for evaluation and guidance. This could be a sign that your COPD is progressing or that another underlying issue may be affecting your breathing.
Your healthcare provider can assess your symptoms, conduct necessary tests, and adjust your treatment plan accordingly to help improve your breathing and quality of life. They may recommend adjustments to your medication regimen, suggest pulmonary rehabilitation programs, or provide other interventions tailored to your specific needs.
It's important not to ignore worsening shortness of breath as it can indicate a decline in lung function.
In the next section about 'weight management,' we will explore how maintaining a healthy weight can positively impact COPD symptoms and overall respiratory health.
Weight management
Making healthy lifestyle choices and maintaining a balanced diet are essential to managing our weight effectively. Here are three key strategies to support weight management for individuals with COPD:
Portion control: Pay attention to portion sizes and aim for smaller, more frequent meals throughout the day. This can help prevent overeating and reduce feelings of breathlessness during meal times.
Nutrient-rich foods: Focus on consuming nutrient-dense foods such as fruits, vegetables, whole grains, lean proteins, and low-fat dairy products. These provide essential vitamins, minerals, and fiber while lowering calories.
Regular physical activity: Engage in regular exercise suitable for your fitness level. Walking or light aerobic exercises can improve lung function and promote weight loss.
By implementing these strategies into our daily routine we can effectively manage our weight. Positive lifestyle changes improve overall health and well-being while mitigating the effects of COPD.
The next section will discuss how we can further manage COPD at home without compromising our quality of life.
How can I manage COPD at home?
To manage COPD at home, we can focus on implementing certain lifestyle changes and incorporating self-care practices.
First and foremost, quitting smoking is important if you haven't already done so. Smoking worsens COPD symptoms and speeds up the progression of the disease.
Maintaining a healthy weight through proper nutrition and regular exercise can help improve lung function and overall well-being.
It's also crucial to avoid exposure to lung irritants such as secondhand smoke, air pollution, and chemical fumes.
Practicing good hygiene, washing hands frequently, and getting vaccinated against respiratory infections like the flu and pneumonia can also help prevent developing or exacerbating COPD.
By taking these steps, you can actively manage your COPD at home and improve your quality of life.
Now let's move on to how COPD is diagnosed.
How is COPD diagnosed?
To diagnose COPD, your healthcare provider will consider your medical history, conduct a physical exam, and order diagnostic tests such as spirometry and imaging.
During the medical history evaluation, they will ask about your symptoms, smoking history, exposure to lung irritants, and any family history of lung disease.
The physical exam will involve listening to your lungs with a stethoscope and checking for signs of respiratory distress.
Spirometry is a common test that measures how much air you can inhale and exhale forcefully.
Imaging tests like chest X-rays or CT scans can help assess the condition of your lungs.
These tests are essential in determining if you have COPD and its severity.
Now let's discuss COPD's stages and how they affect treatment options.
What are the stages of COPD?
The stages of COPD range from mild to severe and help determine the appropriate treatment options. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) has classified COPD into four stages based on the severity of symptoms and lung function.
In stage 1, also known as mild COPD, airflow limitation is present, but symptoms may not be noticeable yet.
Stage 2, or moderate COPD, is characterized by a worsening airflow limitation and the onset of symptoms such as coughing and shortness of breath.
Stage 3, or severe COPD, involves further deterioration in lung function and increased limitations in daily activities.
Finally, stage 4, also known as very severe COPD, is marked by severely reduced lung function and significant impairment in quality of life.
Understanding the stage of COPD helps healthcare providers develop an individualized treatment plan tailored to each patient's needs.
Now let's move on to learn about Salla disease.
Salla disease
Now, let's focus on another lung disease called Salla disease. Salla disease is a rare genetic disorder that affects the metabolism of sialic acid, leading to the accumulation of this substance in the body. This condition primarily affects the nervous system and can cause developmental delays, movement difficulties, muscle weakness, and intellectual disability.
Salla disease is typically diagnosed in infancy or early childhood based on clinical symptoms, genetic testing, and imaging studies. Unfortunately, there is currently no cure for Salla disease. Treatment mainly focuses on managing symptoms and providing supportive care.
Understanding rare diseases like Salla is crucial as it allows us to provide better support and resources for individuals with these conditions.
Now let's transition into the next section, where we will discuss mild COPD (stage 1 or early stage) and its management strategies.
Mild COPD (stage 1 or early stage)
If you have mild COPD (stage 1 or early stage), effective management strategies are available to help you control your symptoms and improve your quality of life.
The first step is to quit smoking if you haven't already, as it is the most important thing you can do to slow down the progression of COPD. Avoiding lung irritants such as secondhand smoke and air pollution is also essential.
Regular exercise, including walking or swimming, can help strengthen your lungs and improve your overall fitness. Your healthcare provider may also prescribe medications such as bronchodilators or inhalers to help open up your airways and make breathing easier.
By taking these steps and working closely with your healthcare team, you can effectively manage your mild COPD and continue living a fulfilling life.
Moving on to moderate to severe COPD (stages 2 and 3),...
Moderate to severe COPD (stages 2 and 3)
Moving on from discussing mild COPD, let's focus on moderate to severe COPD, which corresponds to stages 2 and 3. At this stage, individuals may experience more frequent and severe symptoms that significantly impact their daily lives.
Shortness of breath becomes more pronounced, even with minimal physical activity. Coughing and wheezing become more persistent, and exacerbations or flare-ups occur more frequently. Managing these symptoms becomes crucial to maintain a good quality of life.
Regarding treatment options, medications such as bronchodilators and glucocorticosteroids are commonly prescribed to help alleviate symptoms and prevent exacerbations. Oxygen therapy may also be necessary if blood oxygen levels are low. Lifestyle changes continue to play an important role in managing the condition, including quitting smoking and maintaining a healthy diet.
Now that we have explored moderate to severe COPD let's delve into the final stage - very severe COPD (stage 4) - where individuals face even more significant challenges in their respiratory function.
Very severe COPD (stage 4)
To manage very severe COPD, it's crucial to understand the challenges individuals face in their respiratory function at stage 4. At this stage, lung function is significantly impaired, making breathing extremely difficult. People with severe COPD may experience constant shortness of breath, even at rest, and have limited physical activity tolerance. They may require supplemental oxygen therapy around the clock and may be more prone to frequent exacerbations and respiratory infections.
To improve quality of life and prevent further complications, individuals with severe COPD should work closely with healthcare professionals to develop a comprehensive treatment plan tailored to their needs. This may include medication adjustments, pulmonary rehabilitation programs, regular check-ups, and lifestyle modifications to avoid triggers like smoking or pollution.
Moving forward into the next section about 'How can I avoid COPD?', let's explore some preventive measures to help reduce the risk of developing this debilitating condition.
How can I avoid COPD?
To avoid developing COPD, taking preventive measures and making lifestyle choices that minimize the risk factors is important. Here are some steps you can take:
Quit smoking: This is the most effective way to prevent COPD. Seek support from friends, family, or a healthcare professional to help you quit.
Avoid lung irritants: Avoid secondhand smoke, air pollution, and chemical fumes.
Practice good hygiene: Wash your hands frequently to reduce the risk of respiratory infections.
Get vaccinated: Annual flu shots and pneumonia vaccines can help protect against infections that can worsen COPD.
Following these preventive measures can significantly decrease your chances of developing COPD.
However, if you already have COPD, it's important to watch for signs of infection as they can exacerbate your condition.
Why should people with COPD watch for signs of infection?
Pay attention to signs of infection if you have COPD, as they can worsen your condition. People with COPD are more susceptible to respiratory infections due to the weakened state of their lungs. Infections like pneumonia or bronchitis can cause a flare-up in symptoms and lead to further lung damage.
It is important to watch for warning signs such as increased coughing, mucus color or thickness changes, fever, chest pain, and shortness of breath. If you experience any of these symptoms, it is crucial to seek medical attention promptly. Early treatment can help prevent complications and manage the infection effectively.
Understanding the warning signs of infection is essential for individuals with COPD to take appropriate action and maintain their respiratory health.
What are the warning signs of an infection, especially if I have chronic obstructive pulmonary disease?
Watch out for warning signs of infection, such as increased coughing, mucus color or thickness changes, fever, chest pain, and shortness of breath, especially if you have COPD. It is crucial to be vigilant and seek medical attention promptly if you experience any of these symptoms.
Infections can be particularly dangerous for individuals with COPD because they can exacerbate their already compromised lung function. To help you stay informed and take proactive measures, here are four key warning signs to watch for:
Increased coughing: If your cough becomes more frequent or intense than usual, it may indicate an underlying infection.
Changes in mucus: Pay attention to any changes in the color or thickness of your mucus. Yellow or greenish mucus may suggest an infection.
Fever: A persistent fever could signify that your body is fighting off an infection.
Chest pain and shortness of breath can occur when an infection affects the airways and lungs.
Remember, prompt recognition and treatment of infections are vital for managing COPD effectively and maintaining good respiratory health.
Frequently Asked Questions: COPD
To learn more about the COPD found at PlanetDrugsDirect.com, refer to the answers to our frequently asked questions below.
What are the warning signs of an infection, especially if I have chronic obstructive pulmonary disease?
If you have chronic obstructive pulmonary disease (COPD), it's important to be aware of the warning signs of an infection. Common symptoms include increased coughing, changes in the color or amount of mucus, fever, chest congestion, and difficulty breathing.
If you experience any of these symptoms and if they worsen or persist, it is essential to seek medical attention promptly. Infections can exacerbate COPD symptoms and lead to serious complications, so early detection and treatment are crucial for managing your condition effectively.
How can I manage COPD at home?
To manage COPD at home, we can take several important steps:
First and foremost, quitting smoking is crucial if you haven't already.
Avoiding lung irritants like secondhand smoke and air pollution is also essential.
Regular exercise and a healthy diet can help improve lung function and overall well-being.
It's important to follow medication regimens as your healthcare provider prescribes and seek their guidance for any concerns or worsening symptoms.
Why should people with COPD watch for signs of infection?
People with COPD should watch for signs of infection because their compromised lung function makes them more susceptible and vulnerable to further complications. Infections can worsen COPD symptoms and lead to even more serious conditions like pneumonia, which can be life-threatening.
It is important to seek medical attention if there are any signs of infection, such as increased coughing, changes in the color or amount of mucus, fever, or shortness of breath. Early detection and treatment of infections can help prevent further lung damage and improve outcomes for people with COPD.
When should I call my healthcare provider if I have COPD symptoms?
If you have COPD symptoms, calling your healthcare provider when you experience worsening symptoms or signs of infection is important. These may include increased shortness of breath, persistent cough with colored mucus, chest pain, fever, or flu-like symptoms.
Your healthcare provider can evaluate your condition and provide appropriate guidance and treatment. Remember to seek emergency care if you have severe difficulty breathing or talking.
Don't hesitate to reach out for help when needed.
How can I avoid COPD?
To avoid COPD, we can take several steps.
First and foremost, it's important to quit smoking and avoid exposure to secondhand smoke.
We should also avoid environments with poor air quality and harmful particles like dust and chemical fumes.
Regular handwashing and good hygiene can help prevent respiratory infections that could worsen COPD symptoms.
Annual flu shots and the pneumonia vaccine are also recommended for added protection.
Taking these preventive measures can reduce our risk of developing COPD.
Buy COPD Drugs and Medications
We learned about chronic obstructive pulmonary disease (COPD) and its impact on individuals.
We discussed the causes of COPD, including smoking, exposure to pollutants, and genetic factors.
We also explored the symptoms and progression of the disease, as well as ways to manage and prevent it.
People with COPD must be aware of the signs of infection due to their weakened immune systems.
By understanding COPD and taking proactive measures, we can strive to improve our quality of life while living with this chronic condition.





