Waging war on bacterial infections for Disease Control
Fight infections with affordable antibacterial medication from PlanetDrugsDirect. Utilizing our established network of trusted pharmacies, we are able to securely ship affordable antibacterial medications like Cefzil, Keflex, and Tobrex to the United States and across the world. And with our simple prescription upload process, we make the entire process of purchasing your anti-bacterial medication as easy as possible. Browse our selection of effective antibacterial medicines today.
In the vast battle against bacterial infections, antibiotics stand as the towering fortress, safeguarding human health. Just like knights defending their kingdom, antibiotics possess weapons to combat these microscopic invaders. Antibacterial medications are a diverse group of pharmaceuticals designed to target and eliminate bacteria that cause various illnesses. They act as fearless warriors, disrupting vital processes within bacterial cells and crippling their ability to increase and spread disease. However, this noble fight is not without its challenges.
The responsible use of antibacterial medications is paramount in maintaining their efficacy over time. The alarming rise of antibiotic resistance has become an impending threat, reminiscent of a cunning enemy infiltrating the castle walls undetected. This phenomenon occurs when bacteria adapt and develop mechanisms to render antibiotics ineffective, rendering our once mighty defenses impotent.
To ensure victory in this ongoing war against bacterial infections, understanding the different types of antibacterial medications and their mechanisms of action is essential. By grasping the importance of responsible antibiotic use and combating antibiotic resistance collectively, we can fortify our defenses and strive toward a future where bacterial infections are no longer insurmountable obstacles but mere skirmishes on humanity’s path to wellness.
Key Takeaways
Antibiotics are pharmaceuticals designed to eliminate bacteria and disrupt their vital processes.
Antibiotic resistance occurs when bacteria develop mechanisms to render antibiotics ineffective.
Different antibacterial medications have specific mechanisms of action, such as interfering with cell wall or protein synthesis.
Responsible use of antibiotics, education, surveillance, and research is essential in combating antibiotic resistance.
Effective medicines are available, at least at this time, to combat bacterial infection.
Commonly Prescribed Medications
What are Bacteria?
Bacteria are defined as prokaryotic microorganisms, which unlike cells, they lack a distinct nucleus and other organelles due to their lack of internal membranes. Bacteria are considered to be the first organisms that evolved on earth 3.5 billion years ago. Typically, bacteria need a host to grow, obtaining their energy from sugars, proteins and fats.
How do Bacteria Make Us Sick?
Through introduction into our bodies, bacteria make us ill by reproducing, causing sickness by excreting toxins that can affect certain tissues or organs in our bodies. Such ailments are commonly referred to as bacterial infections. Our bodies react to bacterial infections by stimulating our immune system to produce antibodies and other cells to attack the invader.
How Are Bacterial Pathogens Spread?
Bacterial-related infections spread themselves in numerous ways; through the air, with direct contact with infected skin or mucous membranes, indirect contact with contaminated surfaces, or through vector-borne infections from insects including mosquitoes, fleas or ticks.
What Type of Ailments are caused by Bacterial infection?
Bacterial-related afflictions can be acute or chronic in nature. Acute symptoms are those that appear suddenly, and which last for a short period of time while chronic conditions are long-term, persistent, and which may worsen over time. Some related conditions are relatively minor while others may be more serious infections. Below are a number of bacterial infectious diseases along with their symptoms;
Urinary tract infections, or UTIs, affect any part of the urinary system, including the kidneys, ureters, bladder and urethra. UTIs are common infections when bacteria, from the skin or rectum, enter the urethra. Symptoms include pain or a burning sensation during urination.
Tuberculosis (TB) is a bacteria-caused contagious infection that primarily affects the lungs but can migrate to bones, the brain and spine. TB advances in stages, starting with minor indicators including a low fever, tiredness and cough, to later, more pronounced symptoms including chills, weight loss, night sweats, and loss of appetite. Final stages can include chest pain, sudden and severe headaches, confusion, seizures, coughing up blood, or blood appearing in the urine or stool. Urgent care should be sought if one experiences any of the latter symptoms.
Pneumonia is an infection of the air sacs in one or both lungs. Symptoms include severe cough with phlegm, fever, chills and breathing difficulties. According to a 2020 National Hospital Ambulatory Care Survey, 1.5 million visits to emergency departments as a result of pneumonia were reported in America.
Syphillis is a highly contagious sexually transmitted bacterial infection which manifests in painless sores on the genitals, rectum or mouth. The condition spreads through contact with an already infected person. The infection is treatable with medication. If untreated, syphilis can cause serious health problems including permanent brain, heart, muscle, bone and eye damage. To reduce exposure to syphilis the use of a condom during sex is recommended.
Lyme Disease is a relatively rare condition which is transmitted through tick bites. Symptoms usually take three to 30 days to manifest and include rashes, fever, chills, fatigue and headaches. Late-stage Lyme disease can also cause hand and leg numbness, arthritis and short-term memory loss. Antibiotics are usually prescribed to treat the condition.
Meningitis is an infection, causing inflammation of the meninges which is the protective tissue which surrounds and protects the brain and spinal cord. The condition is serious and immediate medical attention should be sought during its onset. Unchecked meningitis can cause death. The route of transmission varies and can be spread by raspatory droplets or throat secretions. Some bacteria which carry meningitis often reside in the human gut or vagina and can spread from mother to child during birth. Symptoms include headache with nausea or vomiting, decreased appetite, confusion, sudden fever, seizures, sensitivity to light, sleepiness, lethargy and skin rashes.
Chlamydia is a bacteria-caused, common sexually transmitted infection. Initial stages reveal no symptoms, but health related problems can arise in later stages. Symptoms in women can include vaginal discharge, itching in the vaginal area, bleeding between periods and painful sexual intercourse. Common symptoms for men may include pain and swelling in the testicles, penis discharge, pain while urinating, lower abdomen or rectal pain and bleeding. Untreated chlamydia can lead to a number of serious, even deadly conditions including sterility, pelvic inflammatory disease and prostatitis.
Strep throat is also a bacterial infection and manifests as a sore and scratchy throat. Sore throats can manifest as a result of many causes and strep only accounts for a small portion of these. Accompanying symptoms often include painful swallowing, red and swollen tonsils, tiny red spots at the back of the mouth, tender lympth nodes, fever, headache, rash and body aches. Regular hand washing and sanitizing, covering one's mouth when coughing or sneezing and non-sharing of drinking glasses or food utensils are effective measures to prevent strep infection. Antibiotics are usually prescribed to treat strep throat.
What Prevents our Bodies from Being Able to Combat Bacteria?
Germs, or microbes, are everywhere - in the air, on food, plants, animals, in the soil and water and on practically every surface including our bodies. Most microbes are harmless, and our immune system generally protects us from more harmful strains. However, some microbes are constantly mutating, and some even develop antimicrobial resistance - or in other words, resistance to human immune reactions, and more concerning, resistance to antibiotics. Because bacteria are able to mutate in response to immune reaction, these microbes can create defenses against our body's immune responses. In such cases we often employ antibiotics, but as their use becomes ubiquitous, microbes are showing an astonishing ability to adapt, and potentially defeat the effects of antibiotics. Before we examine the potential dangers that antibiotic-resistant bacteria strains pose, let's look at some types of medications that are used to fight bacterial infections.
Types of Antibacterial Medications
Various classes of antibacterial medications are available, each with different mechanisms of action and targets within bacterial cells.
These antibacterial drugs, also known as antibacterial medicine or antibacterial meds, are designed to specifically target bacteria and inhibit their growth or kill them entirely.
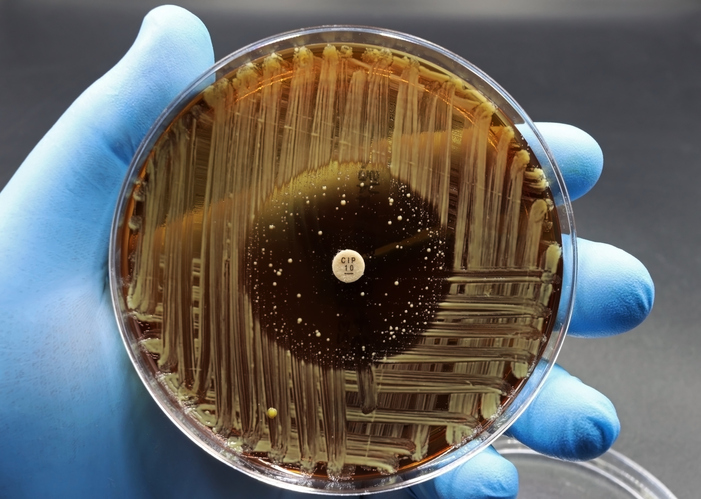
Some standard classes include beta-lactams, which interfere with bacterial cell wall synthesis; macrolides, which inhibit protein synthesis by binding to the bacterial ribosome; and fluoroquinolones, which interfere with DNA replication in bacteria.
Other classes, such as tetracyclines, sulfonamides, and aminoglycosides, have different modes of action targeting bacterial metabolism or protein synthesis.
Understanding the mechanisms of action of these different classes is crucial for determining appropriate treatment options for specific infections.
Popular Anti-bacterial Medications Found at PlanetDrugsDirect.com
PlanetDrugsDirect.com carries a full range of antibacterial drugs, from Achromycin, Doryx, Mycobutin, Valtrex to Surolan, Tobrex, and Vigamox. For a complete listing of all antibacterials that PlanetDrugsDirect.com carries, and to get great savings on your next prescription purchase, please visit this catalog page.
Mechanisms of Action
Mechanisms of action for antibacterial medications involve targeting specific components within bacterial cells, such as cell walls or protein synthesis, to disrupt their normal functioning. By inhibiting cell wall synthesis, antibiotics like penicillin prevent bacteria from maintaining their structural integrity and ultimately cause cell lysis.
Other antibiotics, such as tetracycline and erythromycin, interfere with protein synthesis by binding to the ribosomes responsible for translating genetic information into proteins. These mechanisms effectively kill or inhibit the growth of bacteria and are crucial in treating various bacterial infections.
However, the effectiveness of antibacterial medications is increasingly threatened by antibiotic resistance. Research has shown that 80% of bacteria have developed resistance to at least one type of antibacterial medication. This arises due to selective pressure on bacteria exposed to antibiotics over time, leading to the survival and proliferation of resistant strains.
To address this issue, we must understand the importance of responsible use and develop strategies for combating antibiotic resistance.
Importance of Responsible Use
Responsible use of antibacterial agents is essential for addressing the growing threat of antibiotic resistance, and to ensure the long-term efficacy of these crucial medications. Antibiotic resistance occurs when bacteria develop mechanisms to counteract the effects of antibiotics, rendering the treatments ineffective. This phenomenon is primarily driven by overuse and misuse of antibiotics, such as taking them unnecessarily for viral infections or not completing an entire course of treatment.
The consequences of antibiotic resistance are severe, leading to increased morbidity, mortality, and healthcare costs. To combat this issue, it is imperative that healthcare professionals educate patients about the appropriate use of antibiotics, prescribe them only when necessary, and adhere to guidelines for dosage and duration.
Additionally, promoting research into new drugs and alternative treatments can help mitigate the development and spread of antibiotic resistance. By implementing responsible practices in antimicrobial therapy, we can safeguard the effectiveness of these life-saving medications for future generations.
Combating Antibiotic Resistance
To address the growing threat of antibiotic resistance and to safeguard public health, it is crucial to implement comprehensive strategies that promote responsible use of antibiotics while concurrently investing in research for new treatments.
Enhancing surveillance systems: Strengthening global surveillance networks can enable early detection and tracking of resistant bacteria, helping to identify emerging threats and to inform appropriate response measures.
Improving infection prevention and control: Implementing stringent hygiene practices in healthcare settings can minimize the spread of resistant infections, reducing the need for antibiotics.
Educating healthcare professionals and the public; Raising awareness about appropriate antibiotic use through educational campaigns can empower individuals to make informed decisions when seeking medical care.
Encouraging the development of alternative treatments: Investing in research for novel therapies, such as phage therapy or immune-based approaches, can provide alternatives to traditional antibiotics, potentially reducing reliance on them.
By implementing these strategies, we can combat antibiotic resistance effectively while ensuring effective treatment options remain available for future generations.
Frequently Asked Questions
What are some common side effects of antibacterial medications?
Common side effects of antibacterial medications include nausea, vomiting, diarrhea, and allergic reactions. Antibiotics may also cause disruptions to the average balance of bacteria in the body, leading to conditions such as yeast infections or antibiotic-associated diarrhea.
Can I take over-the-counter pain relievers with antibacterial medications?
Yes, over-the-counter pain relievers can generally be taken with antibacterial medications. However, it is always advisable to consult a healthcare professional or read the medication labels for potential interactions or contraindications.
Are there any natural alternatives to antibacterial medications?
Natural alternatives to antibacterial medications include essential oils (such as tea tree oil and oregano oil), honey, garlic, and probiotics. These substances have shown some antimicrobial properties in laboratory studies, but more research is needed to determine their effectiveness in clinical settings.
How long should I take an antibacterial medication for it to be effective?
To ensure the effectiveness of antibacterial medication, following the prescribed duration of treatment is crucial. The length of treatment varies depending on the type and severity of infection and should be determined by a healthcare professional.
Can I stop taking an antibacterial medication once my symptoms improve?
It is generally recommended to complete the entire course of antibacterial medication as your healthcare provider prescribes, even if your symptoms improve. The goal is to kill bacteria. This helps ensure that all bacteria are eradicated and reduces the risk of bacterial resistance to antibiotics.
What is Gram Negative Bacteria?
To classify bacteria, a process called Gram staining is used. Gram negative bacteria are those which stain red with Gram positive types staining blue. When diagnosing a patient's condition, the Gram test assists healthcare providers to identify which bacteria is present and which type of antibiotics to prescribe to combat them.
Conclusion; Simple Preventative Measures and Plans for Moving Forward
What follows is a concerning warning from the World Health Organization, which should give us pause when approaching the health concerns surrounding bacterial infections, and how we can all implement relatively simple daily procedures to help stop the creeping ineffectiveness of antibiotics;
"The world urgently needs to change the way it prescribes and uses antibiotics. Even if new medicines are developed, without behavioral change, antibiotic resistance will remain a major threat. Behavior changes must also include actions to reduce the spread of infections through vaccination, hand washing, practicing safer sex, and good food hygiene."






